Life isn’t easy for a child born with Dravet syndrome—a rare and devastating form of epilepsy. Many children with Dravet experience hundreds of seizures a day. Few will attend school. Most will never live independently, never drive a car nor attend college, never get a job nor create a family of their own. It’s a life of limits and obstacles—and in many cases, death.
This may be where the story starts. But thanks to the pioneering research taking place at Phoenix Children’s, it’s no longer where the story has to end. From Dravet to muscular dystrophy and more, doctors here are helping kids reclaim the futures they deserve.
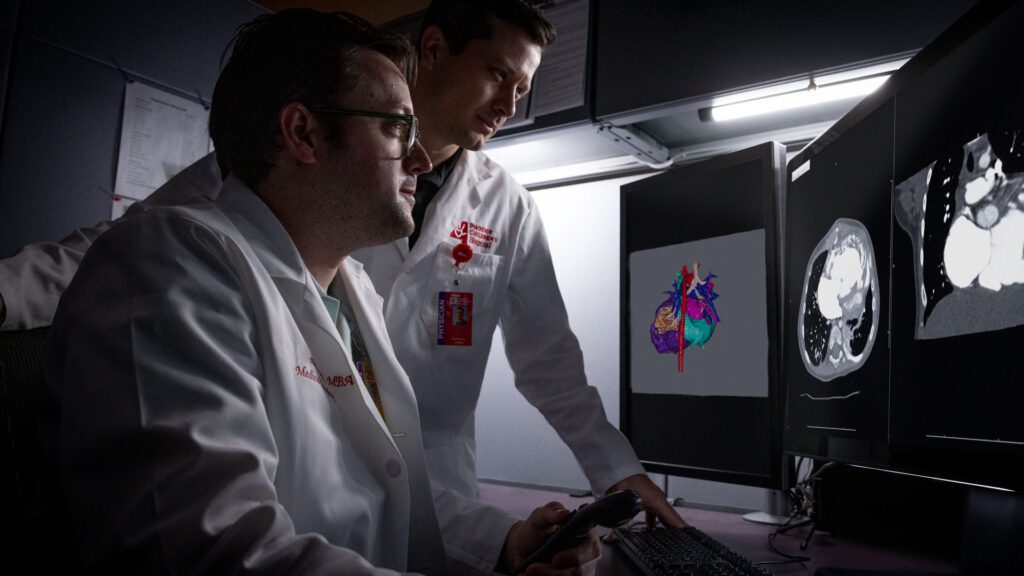
Phoenix Children’s is currently leading or participating in multiple genetic therapy trials, each one focused on treating or even reversing a rare childhood condition. And behind each of those trials is a physician who is determined to do more—for patients, families and pediatric medicine.
Here’s a look at three of those doctors, and the lifechanging work they’re leading.
EPILEPSY: DR. ANGUS WILFONG This new therapy doesn’t just manage seizures—it targets the gene behind them.
Phoenix Children’s is one of 20 sites in the U.S. soon to conduct a trial of a first-in-the-world genetic therapy for epilepsy. This research focuses on one of the most devastating forms of the disease: Dravet syndrome.
Dravet is a genetic condition caused by a mutation in the SCN1A gene. Symptoms appear in the first year of a child’s life, and the condition is highly resistant to medication. It also carries the highest mortality rate of all forms of epilepsy.
That’s why Dr. Angus Wilfong— division chief of neurology and the Dr. Jerry Cox Endowed Chair in Neurology—is so eager to get this trial off the ground.
“There are hundreds of different genetic forms of epilepsy,” he says.
“And there’s active gene discovery work to see if we can treat those other forms. But Dravet is the one that makes the most sense because it’s one of the most catastrophic and deadly forms of epilepsy.”
- “Genetic therapies aren’t just treating the symptoms of disease— they’re getting at the underlying cause of disease.”Angus Wilfong, MDDivision Chief of Neurology; Dr. Jerry Cox Endowed Chair in Neurology
Here’s how the therapy works: SCN1A is known as an autosomal dominant gene, meaning a child typically has one normal copy of the gene and one mutated copy. The problem is that the normal gene copy can’t produce enough sodium channels by itself for proper brain signaling, leading to frequent, uncontrollable seizures.
This trial won’t replace the faulty gene—SCN1A is too large to replace—but it will use synthetic genetic material called antisense oligonucleotides (ASOs) to amplify the healthy gene’s protein production. In other words, the therapy helps the body produce more of what it needs, even if one gene copy is damaged.
Phoenix Children’s has identified 20 eligible patients to participate in this yearlong trial, which will include three to four ASO treatments delivered through a spinal tap, or lumbar puncture.
“Genetic therapies aren’t just treating the symptoms of disease— they’re getting at the underlying cause of disease,” Dr. Wilfong says. “If successful, this therapy will completely change the future for children with Dravet.
“Anyone can follow medicine,” he adds. “But it’s exciting and important for Phoenix Children’s to be leading medicine—and having others follow because we’re making new discoveries that haven’t existed before.”
NEURODEVELOPMENTAL DISORDERS: DR. MICHAEL KRUER A bold new approach silences the genes behind rare brain disorders—offering real hope for patients once out of options.
Thanks to a $750,000 grant from the Arizona Biomedical Research Centre, Michael Kruer, MD, is tackling neurodevelopmental disorders (NDDs) in innovative ways.
A pediatric neurologist and human geneticist, Dr. Kruer serves as the director of Neuroscience Research at Barrow Neurological Institute at Phoenix Children’s. As part of a three-year collaborative project with the n-Lorem Foundation and Columbia University, the team is developing first-inkind antisense oligonucleotides (ASOs)— modified DNA-like molecules—to silence faulty genes behind NDDs such as autism, cerebral palsy and intellectual disability.
“Imagine if we had something that could not just ‘band-aid’ symptoms, but actually counteract what goes wrong at the core of an NDD? It’s remarkable to even consider,” Kruer says. The potential benefits from ASOs are significant: improvements in language, physical abilities, social interaction, seizure control and cognitive ability—things never before possible.
Our genomes serve as a recipe book for how our bodies grow and function, written in the DNA code. Many NDDs stem from single-gene mutations, though different genes can lead to an NDD.


“When we can identify the genetic cause for a disorder, then we can act at the gene level to try to reverse it,” Kruer says. “This work is painstaking. It takes tremendous effort. But we have opportunities now that we’ve never had before.”
Most conditions result from de novo mutations—genetic errors that appear in the affected child for the first time, rather than being inherited. These mutations often cause the gene to become abnormally active, derailing typical brain development. “If we can identify the faulty gene—and confirm it is overactive—then we can design a specific ASO to knock it down to a normal level,” Kruer explains. The project represents a partnership between families, academia and n-Lorem to custom design ASOs for select NDD patients at Phoenix Children’s who share specific gene mutations.
The team hopes that successes with these “pioneer patients” will feed forward so ASOs can be offered to many more patients at Phoenix Children’s—and beyond.
Kruer’s team benefits from the expertise of n-Lorem and a unique FDA regulatory pathway designed to allow the treatment of individual patients with ASOs. Using this approach, ASOs are being developed for NDDs for the first time.
As Kruer summarizes: “Cutting-edge work like this is only possible with the amazing team we’ve assembled and support from granting agencies like the ABRC and generous donors. It is our great hope that success during these foundational stages will redefine how NDDs are treated.”
MUSCULAR DYSTROPHY: DR. SAUNDER BERNES What if heart cells could help heal muscle? A pioneering trial explores an uncharted path.
As part of his work at Barrow Neurological Institute at Phoenix Children’s, Saunder Bernes, MD, medical director of the Neuromuscular Program, has been involved with disease-modifying therapies for spinal muscle atrophy (SMA), a rare degenerative disorder of motor neurons. These therapies have not only changed clinical outcomes for patients, but they’ve also resulted in normal motor development with early treatment.
Now, Dr. Bernes is expanding his research to include Duchenne muscular dystrophy (DMD), a condition that causes muscle weakness and shrinking, triggering severe health issues such as immobility and trouble swallowing or breathing.
Affecting 1 in 3,500 to 5,000 boys, DMD is a progressive, genetic neuromuscular disorder caused by mutations to a gene that provides instructions for the body to make a protein called dystrophin. Symptoms appear around the age of 3. The average life span of a patient with DMD is mid to late 20s; death is almost always from cardiac disease.
This is where Dr. Bernes’ current research comes into play.
“The trial that we’re heavily involved in right now is a cell-based therapy,” Dr. Bernes says. “It’s extracting cardiac cells from human cadaver hearts and administering them through a vein in boys with DMD.”
HOPE-3 is a Phase 3 trial—a late-stage study that tests whether a treatment is effective and safe in a larger patient group—in which participants are randomly assigned to receive either the cardiac cells or a placebo for a year. Out of 45 patients nationwide, five are at Phoenix Children’s under the care of Dr. Bernes.
Dr. Bernes explains how it works: “Most people, when they talk about cell-based therapy, think that the cells you’re taking are being incorporated and reproduced. But that’s not the case here. There are cells in human hearts with different forms of micro-RNA. These micro-RNA forms are anti-inflammatory or antifibrotic. We infuse them into the circulation; in the lungs, the cells break apart and release a factor that’s distributed systemically. It’s almost like taking a drug, but the drug is actually cardiac cells from human hearts.”
- “It’s so reassuring to tell a family that their child isn’t going to have significant cardiac disease.”Saunder Bernes, MDMedical Director, Neuromuscular Program
This is an “add-on therapy” to other FDA-approved therapies. At Phoenix Children’s, 25 boys with DMD have received the FDA-approved gene-transfer therapy.
To qualify for the cell-based therapy trial, patients—ambulatory or not—must be between the ages of 10 and 18 and able to travel to the hospital every three months for a year for the intravenous infusions. Dr. Bernes notes that it can be overwhelming for participants. But early data promises good news for patient outcomes.
“Data suggests that cardiac function is significantly improved. If we can improve that, we’re talking about changing the life of a boy who, 10 years ago, might have died before he was 20. I have to say, it’s so reassuring to tell a family that their child isn’t going to have significant cardiac disease.”
WHAT IS GENETIC THERAPY?
An explainer from the experts at Phoenix Children’s
Genetic therapy is a medical approach that aims to treat or even prevent disease by correcting problems at the gene level. These cutting-edge techniques may replace faulty genes, silence harmful ones or help the body make more of a missing protein. Unlike traditional treatments that manage symptoms, genetic therapy targets the root cause of illness. Major types include: • Gene transfer therapy: Introducing a new gene to replace or supplement a faulty one.
• Gene silencing: Blocking the activity of a malfunctioning gene, often using antisense oligonucleotides (ASOs).
• Cell-based therapy: Using healthy donor cells— sometimes modified—to deliver therapeutic effects.
• Gene expression enhancement: Boosting the output of healthy genes. Phoenix Children’s is one of only a handful of pediatric institutions nationwide conducting clinical trials in this emerging field. While still in its early stages, genetic therapy holds the potential to transform how we treat everything from epilepsy to muscular disorders and beyond.
A LOOK AHEAD
Stewart Goldman, MD, senior vice president of research and chair of the Department of Child Health at Phoenix Children’s, says the promise of genetic therapy is profound—but so is the responsibility.
“This is a really important step for the health of children and society,” he says. “But it’s our moral and ethical responsibility to make sure that we do no harm—to make sure that we improve not just the length but the quality of patients’ and families’ lives.”
Dr. Goldman is focused on ensuring that the work never loses sight of the people at its heart. “I want Phoenix Children’s to not only participate but lead,” he says, “yet to do so in a way that never loses sight of the short- and long-term risks.”
To learn how you can help accelerate advancements in gene therapy, please contact Jana Earnest, senior philanthropy officer at Phoenix Children's Foundation, at 602-933-1857 or jearnest@phoenixchildrens.com.