Acute myeloid leukemia (AML) is a roller coaster of a diagnosis. While treatment is often successful and remission rates are relatively high, relapse is all too common. And the disease’s survival rate—which is about 60% to 70% in patients under 20—is well below where it needs to be.
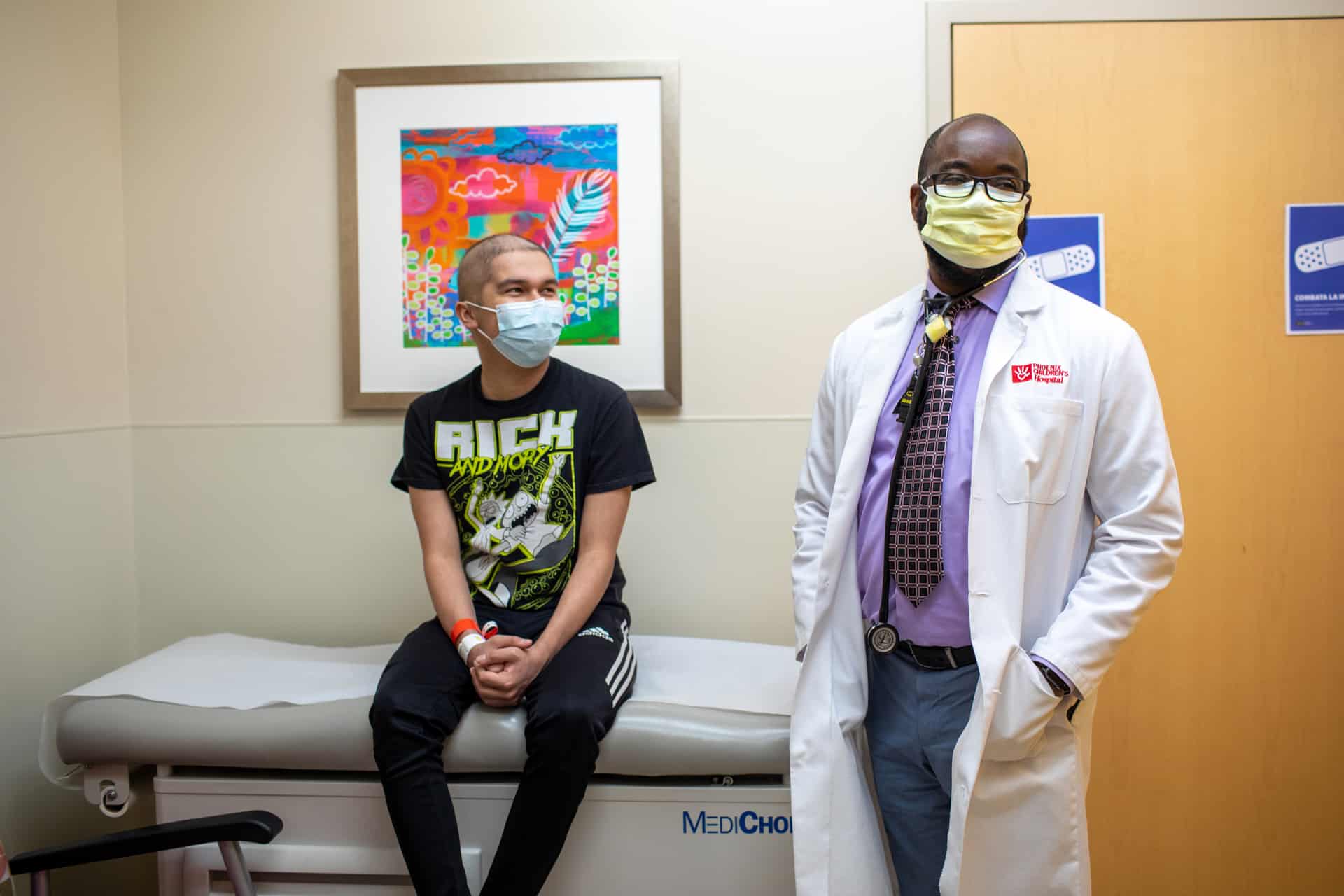
Fortunately, Phoenix Children’s hematologist-oncologist Dr. Alexander Ngwube is working to change that. With a $250,000 grant from Jeff Gordon Children’s Foundation, Dr. Ngwube’s research is about to step on the gas against AML recurrences.
About AML
AML accounts for about 20% of all childhood leukemias (cancers that originate in the blood or bone marrow); about 800 cases are diagnosed in the U.S. each year. With AML, the bone marrow, which is responsible for producing new blood cells, makes abnormal white blood cells, red blood cells or platelets that never mature.
The danger of AML is twofold: Not only can the abnormal cells spread to other parts of the body, but the overproduction of abnormal cells means there’s less room for healthy cells. And without a high percentage of normal blood cells, patients are at risk for infection, anemia and bleeding. Treatment for AML in children usually involves chemotherapy and blood stem cell transplant.


Pilot study success
The vast majority (85% to 90%) of AML patients have success with treatment and go into remission. Regular maintenance chemotherapy may be needed to prevent the cancer from coming back. Still, AML returns in about 30% to 40% of children, many of whom end up dying from the disease, which tends to be more aggressive in recurrence.
Dr. Ngwube’s research is aimed at reducing the relapse rate by administering additional stem cells along with the maintenance chemotherapy. Instead of transplanting all the donor cells at once, Dr. Ngwube saves some and transplants them intermittently during remission.
- We went from seeing a leukemia-free survival rate in the range of 60% and 70% to having leukemia-free survival rate in the high 80s to 90s. That's huge.Dr. Alexander NgwubeHematologist-oncologist at Phoenix Children’s
“The idea is that the donor stem cells have more time to mature,” Dr. Ngwube says. “And so they can go about the business of attacking and destroying any leukemic cells that are still hanging around.”
In a pilot study that included 12 patients, Dr. Ngwube saw a 20% reduction in relapse rates using intermittent stem cell therapy. “We went from seeing a leukemia-free survival rate in the range of 60% and 70% to having a leukemia-free survival rate in the high 80s to 90s,” he says. “That’s huge.”


The next phase
Now, with the grant from Jeff Gordon Children’s Foundation, Dr. Ngwube will be expanding his research into a prospective trial in which he’ll recruit 30 patients not only from Phoenix Children’s but also Yale New Haven Children’s Hospital in Connecticut, Mayo Clinic Children’s Center and others.
“I wouldn’t have been able to continue this research without the grant, so I’m very grateful,” Dr. Ngwube says. “But at the end of the day, the people who benefit from these things are the wonderful families that we are privileged to care for.”
You can help our physicians and researchers continue their trailblazing work by supporting the Center for Cancer and Blood Disorders at Phoenix Children’s.
If you have a story about how your life has been touched by Phoenix Children’s, we want to hear from you.